For generations, urinary tract infections, one of the world’s most common ailments, have been easily and quickly cured with a simple course of antibiotics.
But there is growing evidence that the infections, which afflict millions of Americans a year, mostly women, are increasingly resistant to these medicines, turning a once-routine diagnosis into one that is leading to more hospitalizations, graver illnesses and prolonged discomfort from the excruciating burning sensation that the infection brings.
The New York City Department of Health has become so concerned about drug-resistant U.T.I.s, as they are widely known, that it introduced a new mobile phone app this month that gives doctors and nurses access to a list of strains of urinary tract infections and which drugs they are resistant to.
The department’s research found that a third of uncomplicated urinary tract infections caused by E. coli — the most common type now — were resistant to Bactrim, one of the most widely used drugs, and at least one fifth of them were resistant to five other common treatments.
“This is crazy. This is shocking,” said Lance Price, director of the Antibiotic Resistance Action Center at George Washington University, who was not involved in the research.
The drug ampicillin, once a mainstay for treating the infections, has been abandoned as a gold standard because multiple strains of U.T.I.s are resistant to it. Some urinary tract infections now require treatment with heavy-duty intravenous antibiotics. Researchers last year reported in a study that a third of all U.T.I.s in Britain are resistant to “key antibiotics.”
Certainly, the day-to-day experience of having a U.T.I. is growing less routine for many women.
Carolina Barcelos, 38, a postdoctoral researcher in Berkeley, Calif., said she had several U.T.I.s as a teenager, all successfully treated with Bactrim. When she got one in February, her doctor also prescribed Bactrim, but this time it didn’t work.
Four days later, she returned and got a new prescription, for a drug called nitrofurantoin. It didn’t work either. Her pain worsened, and several days later, there was blood in her urine.
Her doctor prescribed a third drug, ciproflaxacin, the last of the three major front-line medicines, and cultured her urine. The culture showed her infection was susceptible to the new drug, but not the other two.
“Next time,” Dr. Barcelos said, “I’m going to ask them to do a culture right away. For eight days I was taking antibiotics that weren’t working for me.”
Usually, it is people with weakened immune systems or chronic medical conditions who are most vulnerable to drug-resistant infections, but U.T.I.s have a dubious distinction: They are the single biggest risk to healthy people from drug-resistant germs.
Resistance to antibiotics has become one of the world’s most pressing health issues. Overuse of the drugs in humans and livestock has caused germs to develop defenses to survive, rendering a growing number of medicines ineffective in treating a wide range of illnesses — a phenomenon that is playing out worldwide with U.T.I.s.
The World Health Organization, while noting that data on urinary tract infections and drug resistance is “scarce,” said the fact the infections were so common strongly suggested that increasing resistance would lead to more severe illnesses and fatalities.
The solution, researchers and clinicians say, includes a continued push for more judicious use of antibiotics worldwide. But more immediately, a partial solution would be the development of quick, cheap diagnostic tools that would allow an instant urine culture so that a doctor could prescribe the right drug for U.T.I.s.

But whether to wait the several days it usually takes to get lab results before prescribing presents a tough dilemma for doctors and patients, who frequently are desperate for relief. Plus, depending on a person’s insurance, getting a culture can be expensive.
Generally doctors still do not order a urine culture before prescribing an antibiotic.
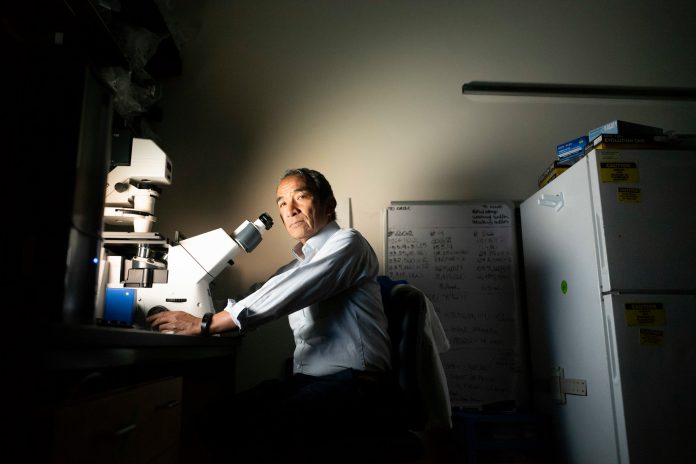
“In the old days, the list of antibiotic options was short but by and large they would all work,” said Dr. James Johnson, an infectious disease professor and leading researcher on urinary tract infections at the University of Minnesota.
Some women have U.T.I.s that the body fights off on its own without using antibiotics, while other women may have a different low-level ailment that feels like a U.T.I., but isn’t. The safest course is to see a doctor and make an informed decision that includes a judicious determination of whether antibiotics are warranted. The science does not support the efficacy of some popular remedies like cranberry juice or cranberry pills.
_______
Officials from the federal Centers for Disease Control and Prevention said that U.T.I.s acquired by otherwise healthy people were a growing concern and one poorly studied. They are not tracked nationally.
In older people, urinary tract infections can be deadly, but tracking in the United States is so weak that there are no reliable estimates on the numbers of deaths related to the infections. The C.D.C. published an estimate of 13,000 per year, but that figure comes from a paper looking at 2002 data and refers only to U.T.I.s acquired in hospitals.
Source: nytimes.com